1801006099 long case
This IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment
Chief Complaints:
A 28 year old male came to OPD with cheif complaints of
Abdominal distension since 10 days
Shortness of breath since 5 days
Yellowish discoluration of eyes since 5 days
Fever since 3 days
Pedal edema_3 days
History of present illness:
Patient was apparently asymptomatic 4 months back then he developed abdomibal distension which is Insidious in onset and gradually progressive . Shortness of breath which is grade 3 ,aggravated on lying down and relived on standing ,yellowish discoloration of eye for 5days , fever which Insidious in onset and gradually progressive is not associated with chills and rigor ,no evening rise of temperature he went to hospital ,
History of similar complaints in the past 4 months back he took medication for that and symptoms subsided
Then ,he started to consume alcohol(180 ml) daily ,
he had same complaints from 10 days he came to hospital
Then he presented on with complains of Abdominal distension since 5days, Shortness of Breath Gradelll ,fever not associated with Chills and rigor without evening rise of temperature, Altered sleep cycle,facial puffiness,, pedal edema is seen for 3 days. Pitting type
No history of palpitions, syncope
No history of decreased urinary output
No history of hematemesis, melena,
Past history:
History of similar complaints in the past 4 months back
Not a known case of diabetes,hypertension,asthma,Tb,CAD.
Personal history:
Diet : Mixed
Appetite : Decreased
Sleep : Disturbed
Bowel and Bladder moments : normal
Addictions : alcohol consumptions daily
Micturition : Normal
Family history:
Not significant.
General physical examination:
Patient is conscious ,coherent and cooperative and well oriented to time, place and person.
moderately built and nourished.
Pallor-absent
Icterus-present
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Edema _ present
Vitals:
Temperature - 98.2*c
PR :- 95bpm
RR :-22cpm
BP :- 130/80mm Hg
SPO2 :- 98%
Systemic examination:
Lips
Teeth
Gingiva
Tongue
Buccal mucosa
All are normal
Abdomen examination:
Inspection:
Shape_distension of abdomen
Flanks _full
Umbulicus_everted
Engorged veins _ present
Skin over abdomen _shiny and Streached
No visible scars and sinuses
No visible peristalsis
Movement of abdomen_moving with respration
No hernial orifice
Palpation:
Abdomen
,non tender.soft,
Uniformly distended
No splenomegaly hepatomegaly
Kidney_not palpable
Percussion:
Fluid thrill_present
Auscultion:
Bowel sound heard
No bruits
Respiratory examination:
-Upper respiratory tract:No DNS,Nasal polyp
Oral cavity:Good oral hygiene.No loss of tooth/caries.
Posterior pharyngeal wall-normal.
-Lower respiratory tract:
On inspection:
Shape of chest: Elliptical,b/l symmetrical chest.
Trachea appears to be central
Chest moves on respiration and equal on both sides
No accessory respiratory muscles are used in respiration.
Apical impulse is not visible.
No scars, sinuses,engorged veins.
No kyphosis, scoliosis.
Palpation:
No local rise of temperature, tenderness.All inspectory findings are confirmed by palpation.
Trachea-central position
Apex beat-5th ICS medial to midclavicular line
Percussion:
Supraclavicular
Infraclavicular
Mammary
Inframammary
Axillary
Infra axillary
Supra scapular
Infra scapular
Inter scapular
Normal Resonance in all areas
Auscultation:
Bilateral air entry present.
Normal vesicular breathe sounds heard.
Cardiovascular examination:
JVP- Not raised,normal wave pattern.
-on inspection:
shape of chest wall elliptical, no visible pulsations, no engorged veins present.
Apical impulse is not visible
Palpation:
apex beat over left 5th intercostal space medial to midclavicular line. No parasternal heaves
No precordial thrill
No dilated veins
Percussion:
Auscultation:s1 and s2 heard no murmurs heard.
CNS EXAMINATION:
Higher mental functions:
Patient is conscious,coherent,cooperative,
Speech and language is normal
CRANIAL NERVES:Intact
Olfactory nerve
Optic nerve
Occulomotor nerve
Trochlear
Trigeminal
Abducens
Facial
Vestibulocochlear
Glossopharyngeal
Vagus
Spinal accessory
Hypoglossal
Motor system:
Right Left
Bulk UL n n
LL n n
Tone UL n n
LL n n
Power UL 5/5 5/5
LL 5/5 5/5
Reflexes:
Superficial reflexes: present
Corneal
Conjunctival
Abdominal
Plantar reflexes
Deep reflexes:Present
Biceps
Triceps
Knee
Ankle
Co ordination present
Gait normal
No involuntary movements
Sensory system:
Pain, temperature, pressure, vibration perceived
Romberg's test:absent
Graphaesthesia:normal
Cerebellar signs:
No nystagmus,Finger nose test positive,Heel knee test positive
No signs of meningeal irritation.
Provisional diagnosis: decompensated liver disease with Ascitis secondary to alcoholic Cirrhosis
Investigations:
ECG:
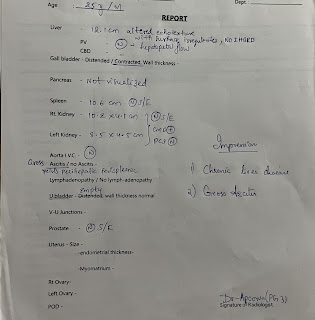
USG:
2D ECHO:
Provisional diagnosis:
Chronic liver disease.
Treatment:
1. FLUID RESTRICTION.
2. SALT RESTRICTED NORMAL DIET.
3. INJ. CEFOTAXIM 2 GRAM TWICE DAILY INTRAVENOUSLY.
4. INJ. VIT K 1 AMP IN 100 ML NS ONCE DAILY INTRAVENOUSLY.
6. INJ. PAN 40 MG TWICE DAILY INTRAVENOUSLY.
7. INJ. ZOFER 4 MG THRICE DAILY INTRAVENOUSLY.
8. TAB. PCM 650 mg SOS (<1 GRAM / DAY).
9. SYP. LACTULOSE 15 ML 30 MINUTES BEFORE FOOD THRICE DAILY.















Comments